The ProRehab Center Blog
Expert Therapists
Innovative Technology
Individualized Plans

Do you have or are dealing with... Difficulty with controlling your bladder or bowels? Pain in and/or around your pelvis or abdomen? Constipation? Pain with sexual activity? Pelvic Organ Prolapse or feeling of pressure and heaviness in your pelvis? Currently pregnant or more than 6-weeks postpartum? If you’ve experienced any of these, just know you aren’t alone! Up to 49% (or more) of individuals, female and male, experience one or more of these symptoms during their lifetime. While this may be common, it doesn’t have to be something you “just deal with” and Pelvic Floor Physical Therapy might be something worth considering! What is Pelvic Floor PT? Pelvic Floor Physical Therapy is a specialized area of PT, encompassing a thorough assessment of the of the body’s functioning in relation to bowel, bladder, sexual health, and movement in our daily lives. Your Physical Therapist has undergone additional hands-on training to specifically examine and treat the muscles and structures in and around the pelvis. Pelvic floor physical therapy is an essential resource for individuals dealing with various pelvic health issues, such as: Bowel or Bladder Incontinence Constipation Diastasis Recti – “separated abdominal muscles or abdominal bloating” Overactive Bladder Pelvis/Perineal pain Pregnancy and Postpartum Hemorrhoids Urinary retention or frequent UTIs/bladder infections Organ Prolapse Coccygodynia - “pain at or around your tailbone” What should I expect during an initial visit? If you’re considering pelvic floor physical therapy (PFPT), the evaluation process might seem a bit daunting. However, it is a crucial step in addressing the issues you may be having and developing the care plan that is best suited to help you •Initial Consultation and Movement Analysis: After spending some time talking with your PT about your symptom presentation, bowel/bladder habits, and medical history, they’ll take some time to look at how your back, hips, knees, core and pelvic floor are moving with daily movements like squatting, bending, sitting, walking, etc. • Physical Assessment: An external and internal examination of your pelvic floor may take place during this first assessment to best observe how your pelvic floor muscles move and function, determine strength, endurance and coordination, and identify if there is any tightness or discomfort of those muscles. *Before starting this portion, your therapist will describe in detail the entire process of the external and internal exam and ensure you know what to expect and that you know you are in control the entire time. They will ask you if you have any questions and confirm you want to proceed with this step. *This does not have to be performed on the first visit, as there are other ways to assess the pelvic floor.* • Goal Setting: At the end of your visit, your PT will then help develop a treatment plan to address any of the limitations or restrictions found during the evaluation to best meet your needs and expected goals. Education on your diagnosis, symptoms, body anatomy and prescribed exercises will also be discussed. You will always have the opportunity to ask questions during your appointments. What are 3 things I can do in the meantime until I come to PT? 1. Be aware of your breathing – try not to hold your breath when picking up things like groceries, your kids, heavy boxes, etc. Remember to take deep breaths to fully fill your lungs (think 360-degree filling of your abdomen, ribs and low back). 2. Stay hydrated – even if you find yourself having to go to the bathroom often, it is important not to limit your fluid intake in order to keep your muscles and joints hydrated. Try to limit beverages with a lot of caffeine, citrus, or carbonation to reduce irritation to your intestines and bladder. 3. Keep moving your body - Gentle movements like walking or yoga are great ways to prompt blood flow to the pelvic area which helps to nourish the muscles and tissues. However, avoid or reduce any overly strenuous activities that can increase tension to the pelvic floor like running or repetitive jumping (just for now!). Your pelvic floor therapist will help assist with returning to these activities that may worsen your symptoms. If Pelvic Floor Physical Therapy is what you're looking for or you aren’t quite sure if the symptoms you’ve been having are related to the pelvic floor, reach out to your doctor or give us a call to set up an appointment today! Annie Foss, PT, DPT
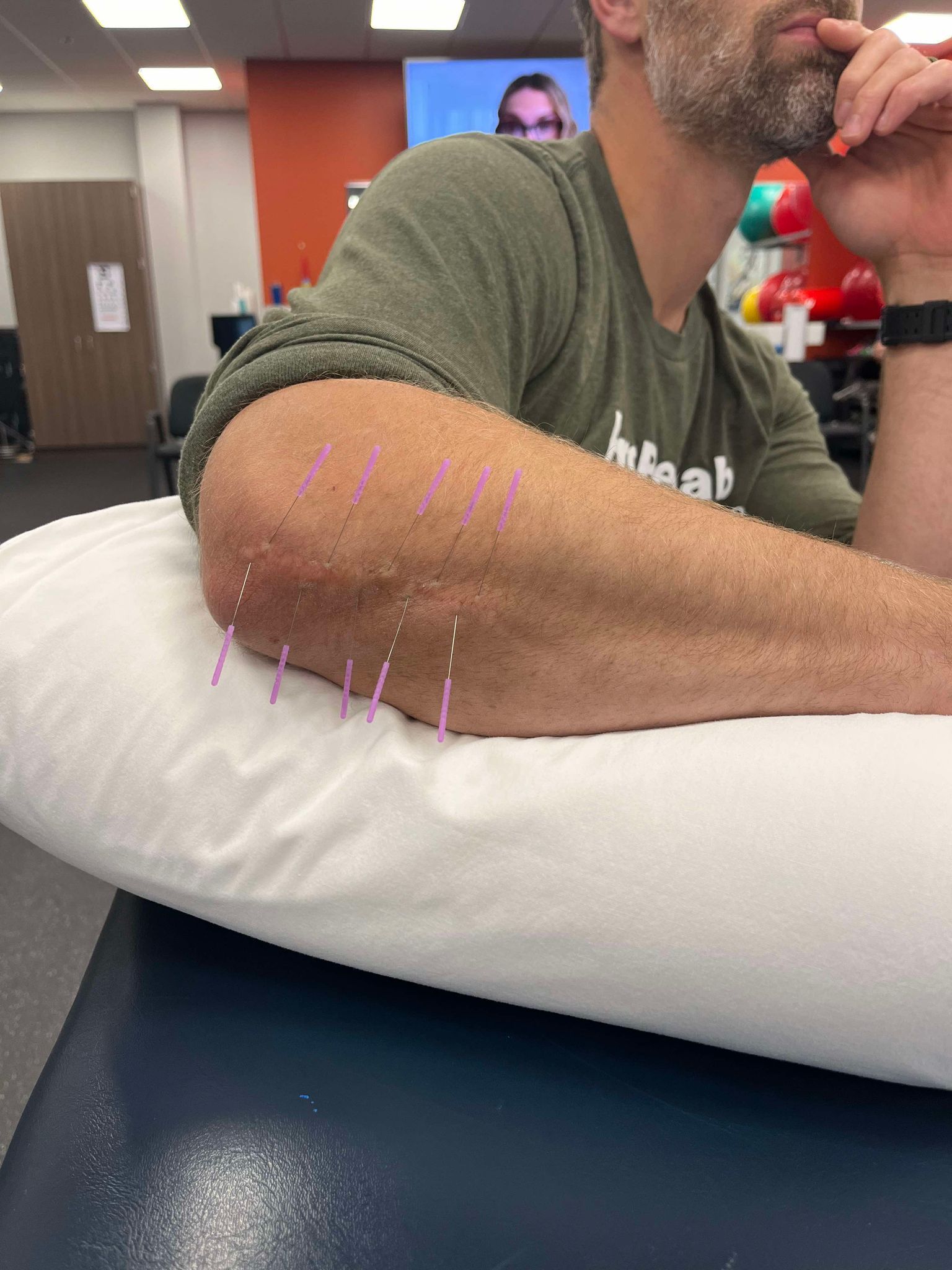
Do you have a scar that didn’t heal right or is painful? Scar formation is a natural process your body goes through when repairing damaged tissue from an injury or surgery. While many wounds heal on their own without issue, some have delayed healing or even get infected. This can result in hypertrophic scars that are painful and don’t move well. They also may have an irregular appearance that can make some people self-conscious. Dry needling, in addition to other physical therapy interventions, can be useful in improving the mobility and overall look of these scars. It can also decrease any pain associated with the scar as well. Dry needling is thought to be the most effective 6 to 18 months after injury due to tissue healing timelines, but it can also be beneficial in decreasing pain beyond that time frame. A well mobile scar allows that area to move more freely and leads to less pain and dysfunction later on in life. If you have a pesky scar that is painful or the appearance bothers you, book a consultation to discuss how dry needling may be beneficial in addressing your concerns. Don’t let scars hold you back from moving optimally! Bridget Juhnke, PT, DPT Sources: Rozenfeld E, Sapoznikov Sebakhutu E, Krieger Y, Kalichman L. Dry needling for scar treatment. Acupunct Med. 2020 Dec;38(6):435-439. doi: 10.1177/0964528420912255. Epub 2020 Mar 30. PMID: 32228036. Chmielewska D, Malá J, Opala-Berdzik A, Nocuń M, Dolibog P, Dolibog PT, Stania M, Kuszewski M, Kobesova A. Acupuncture and dry needling for physical therapy of scar: a systematic review. BMC Complement Med Ther. 2024 Jan 2;24(1):14. doi: 10.1186/s12906-023-04301-4. PMID: 38167051; PMCID: PMC10759514.

Low back pain is one of the most common ailments for seeking out healthcare and affects about 80% of the population at some point in their lifetime. It is the second most common reason for someone to see their primary care provider and accounts for billions of dollars spent annually. Physical therapy is widely considered one of the first, if not the first treatment in managing low back pain. Many episodes of back pain do take care of themselves, but others become chronic (lasting longer than 3 months). As physical therapists, we are often asked, “What can I do for my back pain?” from friends, family, and even just acquaintances when they learn what we do for a living. That answer is difficult to answer since there are many causes of back pain and not all of them are treated the same or with the same exercises. With that said, my most common answer is, “Come in for an evaluation and we can find the best individual exercises for you.” However, some don’t have the time or resources to do that and say so. The next recommendation is activity. General, whole body, free weight strength training has been shown to reduce pain and increase function1. Squats have repeatedly been shown to improve core strength and increase function alone, WHEN DONE CORRECTLY. Squats are one of my favorite exercises, but we see common changes in form and technique, especially with those who have chronic low back pain2. Those individuals would benefit from physical therapy, while others may benefit from a personal trainer as well for coaching on squatting and helping them get set up with an exercise routine (be on the lookout for another blog on correct squat technique and a few of our favorite exercises to improve squats). Another great activity for reducing pain is walking. Walking for 15-20 minutes has been shown to reduce pain and increase reported function in individuals with back pain, especially with chronic back pain. 3 It also is linked with lower stress and temporary reduction in pain. There are even studies on the importance of getting more steps daily following lumbar surgery for predicted long term success.4 My last but not least recommendation is a book called “Treat Your Own Back” by Robin McKenzie (see link below or pick up a copy from our lobby). The book is an easy read and is often read in just a short time. It takes you through self-testing exercises to improve your back pain and is suited for those with chronic or acute back pain. Treat Your Own Back: McKenzie, Robin: 9780987650405: Amazon.com: Books Jon Scherbenske, PT, DPT, Cert-MDT

1. The Mysterious TMJ First things first: What’s the deal with TMJ? It stands for the temporomandibular joint—the hinge that connects your jawbone to your skull. Think of it as the gateway to chewing, talking, and occasionally yelling at slow drivers 😁. When we have dysfunction, we’ll actually call it TMD – temporomandibular dysfunction (but when you come in saying you have TMJ…I get it!). 2. The Drama Queen Joint The TMJ doesn’t like to be overworked or stressed and it lets us KNOW. It throws tantrums in the form of pain, stiffness, and clicks. But we can do something about it! 3. The PT’s Toolbox a. Manual Magic Manual therapy is our secret weapon. We work outside AND inside muscles in order to decrease the tension we’ve been building all day because of life in general. 😊 b. Exercise Yes. We most certainly exercise the jaw and we do it by more than talking (though my twin 6 year old boys think they need to exercise it ALL DAY LONG). We provide different jaw, neck and even upper back exercises to improve posture (see below), stabilize and see those long term results. 4. The Forward Head Posture Conspiracy Your head is like a bowling ball perched on your neck. If it leans forward (thanks, smartphones), your TMJ gets annoyed. It ESPECIALLY gets irritable if we lean forward with our chin in our hand. PTs understand compensation patterns and will get you back on track. 5. The PT-Dentist Tag Team I have worked hard to develop excellent relationships with many of the local dentists and if yours isn’t one of them? I’ll reach out! I do this because we do best if we tag-team this TMJ situation. We chat, we strategize, and we high-five (mentally, of course). Communication is key regarding therapy, benefits of splints, etc. And there you have it! Our whirlwind tour of TMJ treatments. 🦷💪 Sources: Physical Therapy and the TMJ Incorporating Physical Therapy Into Your TMJ Treatment A Proposed Diagnostic Classification of Patients With TMDs Understanding TMJ Disorders and the Role of Physical Therapy Physical Therapy for Temporomandibular Joint Dysfunction (TMJ)



Share On: